Back شذوذ الحركة Arabic Кататония Bulgarian Catatonia (síndrome) Catalan Katatonie Czech Katatoni Danish Katatonie German Katatonio Esperanto Catatonia (síndrome) Spanish Katatonia Basque روانگسیختگی کاتاتونی Persian
| Catatonia | |
|---|---|
| Other names | Catatonic syndrome |
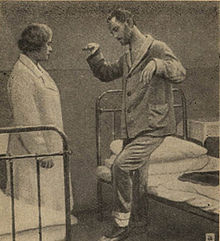 | |
| A patient in catatonic stupor | |
| Specialty | Psychiatry, neurology |
| Symptoms | Immobility, mutism, staring, posturing, rigidity, low consciousness, etc. |
| Complications | Physical trauma, malignant catatonia (autonomic instability, life-threatening), dehydration, pneumonia, pressure ulcers due to immobility, muscle contractions, deep vein thrombosis (DVT)[1] and pulmonary embolism (PE)[1] |
| Causes | Underlying illness (psychiatric, neurologic, or medical), brain injury/damage, certain drugs/medications |
| Diagnostic method | Clinical, Lorazepam challenge |
| Treatment | Benzodiazepines (lorazepam challenge), electroconvulsive therapy (ECT)[1] |
Catatonia is a complex neuropsychiatric behavioral syndrome that is characterized by abnormal movements, immobility, abnormal behaviors, and withdrawal.[2][3] The onset of catatonia can be acute or subtle and symptoms can wax, wane, or change during episodes. It has historically been related to schizophrenia (catatonic schizophrenia), but catatonia is most often seen in mood disorders.[3] It is now known that catatonic symptoms are nonspecific and may be observed in other mental, neurological, and medical conditions. Catatonia is now a stand-alone diagnosis (although some experts disagree), and the term is used to describe a feature of the underlying disorder.[4]
There are several subtypes of catatonia: akinetic catatonia, excited catatonia, malignant catatonia, and delirious mania.[5]
Failure to recognize and treat catatonia may lead to poor outcomes and can be potentially fatal. Treatment with benzodiazepines or ECT can lead to remission of catatonia.[3] There is growing evidence of the effectiveness of the NMDA receptor antagonists amantadine and memantine for benzodiazepine-resistant catatonia.[6] Antipsychotics are sometimes employed, but they can worsen symptoms and have serious adverse effects.[7]
- ^ a b c Balaguer AP, Rivero IS (22 December 2021). "Electroconvulsive therapy, catatonia, deep vein thrombosis and anticoagulant treatment: a case report". General Psychiatry. 34 (6): e100666. doi:10.1136/gpsych-2021-100666. ISSN 2517-729X. PMC 8705197. PMID 35028525.
- ^ Fink M, Taylor MA (1 November 2009). "The Catatonia Syndrome: Forgotten but Not Gone". Archives of General Psychiatry. 66 (11): 1173–1177. doi:10.1001/archgenpsychiatry.2009.141. PMID 19884605.
- ^ a b c Burrow JP, Spurling BC, Marwaha R (2022). "Catatonia". StatPearls. StatPearls Publishing. PMID 28613592.
- ^ Fink M (2011). "Catatonia from its creation to DSM-V: Considerations for ICD". Indian Journal of Psychiatry. 53 (3): 214–217. doi:10.4103/0019-5545.86810. PMC 3221176. PMID 22135438.
- ^ Fink M (July 2009). "Catatonia: A Syndrome Appears, Disappears, and is Rediscovered". The Canadian Journal of Psychiatry. 54 (7): 437–445. doi:10.1177/070674370905400704. PMID 19660165.
- ^ Cite error: The named reference
Carroll-2007was invoked but never defined (see the help page). - ^ Fink M, Taylor MA (2003). Catatonia: A Clinician's Guide to Diagnosis and Treatment. Cambridge University Press. ISBN 978-0-521-82226-8.[page needed]