Back التهاب فرط التحسس الرئوي Arabic Niwmonitis hypersensitifedd Welsh Alveolitis alérgica extrínseca Spanish Pneumopathie d'hypersensibilité French Pneumonite por hipersensibilidade Galician דלקת ריאות מרגישות יתר HE Polmonite da ipersensibilità Italian 過敏性肺炎 Japanese 과민성 폐장염 Korean Allergische alveolitis Dutch
| Hypersensitivity Pneumonitis | |
|---|---|
| Other names | Allergic alveolitis, bagpipe lung, extrinsic allergic alveolitis (EAA) |
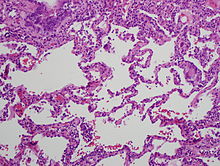 | |
| High magnification photomicrograph of a lung biopsy taken showing chronic hypersensitivity pneumonitis (H&E), showing mild thickening of the walls of the small air sacs by invasion of white blood cells. A multinucleated giant cell, seen within the walls of the air sacs to the right of the picture halfway down, is an important clue to the correct diagnosis. | |
| Specialty | Pulmonology, Occupational Safety and Health, Occupational Medicine, Immunology |
| Symptoms | Dyspnea, fever, chills, cough, fatigue, weight loss |
| Complications | Chronic interstitial lung disease |
| Usual onset | Hours to years depending on type of exposure. |
| Duration | Hours to years depending on type of exposure. |
| Types | Acute, Subacute, Chronic or Fibrotic vs. Non-fibrotic |
| Causes | Variety of respirable antigens found in farming, food processing, handing of animals, and different occupational settings |
| Diagnostic method | Based on home and environmental exposure history taking followed by imaging, spirometry, serology, bronchoscopy, and even lung biopsy. |
| Differential diagnosis | Idiopathic Pulmonary Fibrosis, Occupational asthma, Sarcoidosis |
| Prevention | Avoidance of antigen exposure |
| Treatment | Avoidance of antigen exposure and sometimes steroids |
Hypersensitivity pneumonitis (HP) or extrinsic allergic alveolitis (EAA) is a syndrome caused by the repetitive inhalation of antigens from the environment in susceptible or sensitized people.[1][2] Common antigens include molds, bacteria, bird droppings, bird feathers, agricultural dusts, bioaerosols and chemicals from paints or plastics.[3] People affected by this type of lung inflammation (pneumonitis) are commonly exposed to the antigens by their occupations, hobbies, the environment and animals.[4][3] The inhaled antigens produce a hypersensitivity immune reaction causing inflammation of the airspaces (alveoli) and small airways (bronchioles) within the lung.[4] Hypersensitivity pneumonitis may eventually lead to interstitial lung disease.[5]
- ^ Cite error: The named reference
Sharmawas invoked but never defined (see the help page). - ^ "Hypersensitivity pneumonitis". Nature Reviews Disease Primers. 6 (1): 66. December 2020. doi:10.1038/s41572-020-0207-8. ISSN 2056-676X. PMID 32764556. S2CID 39174418.
- ^ a b Cite error: The named reference
:1was invoked but never defined (see the help page). - ^ a b Quirce S, Vandenplas O, Campo P, Cruz MJ, de Blay F, Koschel D, et al. (June 2016). "Occupational hypersensitivity pneumonitis: an EAACI position paper". Allergy. 71 (6): 765–779. doi:10.1111/all.12866. PMID 26913451.
- ^ Ismail T, McSharry C, Boyd G (May 2006). "Extrinsic allergic alveolitis". Respirology. 11 (3): 262–268. doi:10.1111/j.1440-1843.2006.00839.x. PMID 16635083. S2CID 13460021.