
Back تلين العظام Arabic Osteomalyasiya Azerbaijani Osteomalacija BS Osteomalàcia Catalan نەرمیی ئێسک CKB Osteomalasia Welsh Osteomalazie German Osteomalacia Spanish Osteomalazia Basque نرماستخوانی Persian
| Osteomalacia | |
|---|---|
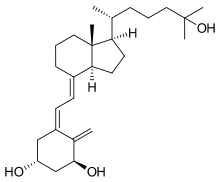 | |
| Cholecalciferol (Vitamin D3), deficiency of which is the most common cause of Osteomalacia | |
| Specialty | Orthopedics |
Osteomalacia is a disease characterized by the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium. The impairment of bone metabolism causes inadequate bone mineralization.
Osteomalacia in children is known as rickets, and because of this, use of the term "osteomalacia" is often restricted to the milder, adult form of the disease. Signs and symptoms can include diffuse body pains, muscle weakness, and fragility of the bones. In addition to low systemic levels of circulating mineral ions (for example, caused by vitamin D deficiency or renal phosphate wasting) that result in decreased bone and tooth mineralization, accumulation of mineralization-inhibiting proteins and peptides (such as osteopontin and ASARM peptides), and small inhibitory molecules (such as pyrophosphate), can occur in the extracellular matrix of bones and teeth, contributing locally to cause matrix hypomineralization (osteomalacia/odontomalacia).[1][2][3][4][5][6][7]
A relationship describing local, physiologic double-negative (inhibiting inhibitors) regulation of mineralization has been termed the Stenciling Principle of mineralization, whereby enzyme-substrate pairs imprint mineralization patterns into the extracellular matrix (most notably described for bone) by degrading mineralization inhibitors (e.g. TNAP/TNSALP/ALPL enzyme degrading the pyrophosphate inhibition, and PHEX enzyme degrading the osteopontin inhibition).[8][9] The Stenciling Principle for mineralization is particularly relevant to the osteomalacia and odontomalacia observed in hypophosphatasia (HPP) and X-linked hypophosphatemia (XLH).
The most common cause of osteomalacia is a deficiency of vitamin D, which is normally derived from sunlight exposure and, to a lesser extent, from the diet.[10] The most specific screening test for vitamin D deficiency in otherwise healthy individuals is a serum 25(OH)D level.[11] Less common causes of osteomalacia can include hereditary deficiencies of vitamin D or phosphate (which would typically be identified in childhood) or malignancy.
Vitamin D and calcium supplements are measures that can be used to prevent and treat osteomalacia. Vitamin D should always be administered in conjunction with calcium supplementation (as the pair work together in the body) since most of the consequences of vitamin D deficiency are a result of impaired mineral ion homeostasis.[11]
Nursing home residents and the housebound elderly population are at particular risk for vitamin D deficiency, as these populations typically receive little sun exposure. In addition, both the efficiency of vitamin D synthesis in the skin and the absorption of vitamin D from the intestine decline with age, thus further increasing the risk in these populations. Other groups at risk include individuals with absorption secondary to gastrointestinal bypass surgery or celiac disease, and individuals who immigrate from warm climates to cold climates, especially women who wear traditional veils or dresses that prevent sun exposure.[12]
- ^ McKee, MD; Buss, DJ; Reznikov, N (13 December 2021). "Mineral tessellation in bone and the stenciling principle for extracellular matrix mineralization". Journal of Structural Biology. 214 (1): 107823. doi:10.1016/j.jsb.2021.107823. PMID 34915130. S2CID 245187449.
- ^ Buss, DJ; Reznikov, N; McKee, MD (1 November 2020). "Crossfibrillar mineral tessellation in normal and Hyp mouse bone as revealed by 3D FIB-SEM microscopy". Journal of Structural Biology. 212 (2): 107603. doi:10.1016/j.jsb.2020.107603. PMID 32805412. S2CID 221164596.
- ^ Salmon, B; Bardet, C; Coyac, BR; Baroukh, B; Naji, J; Rowe, PS; Opsahl Vital, S; Linglart, A; Mckee, MD; Chaussain, C (August 2014). "Abnormal osteopontin and matrix extracellular phosphoglycoprotein localization, and odontoblast differentiation, in X-linked hypophosphatemic teeth". Connective Tissue Research. 55 (Suppl 1): 79–82. doi:10.3109/03008207.2014.923864. PMID 25158186. S2CID 19702315.
- ^ Boukpessi, T; Hoac, B; Coyac, BR; Leger, T; Garcia, C; Wicart, P; Whyte, MP; Glorieux, FH; Linglart, A; Chaussain, C; McKee, MD (21 November 2016). "Osteopontin and the dento-osseous pathobiology of X-linked hypophosphatemia". Bone. 95: 151–161. doi:10.1016/j.bone.2016.11.019. PMID 27884786.
- ^ Barros, NM; Hoac, B; Neves, RL; Addison, WN; Assis, DM; Murshed, M; Carmona, AK; McKee, MD (March 2013). "Proteolytic processing of osteopontin by PHEX and accumulation of osteopontin fragments in Hyp mouse bone, the murine model of X-linked hypophosphatemia". Journal of Bone and Mineral Research. 28 (3): 688–99. doi:10.1002/jbmr.1766. PMID 22991293.
- ^ McKee, MD; Hoac, B; Addison, WN; Barros, NM; Millán, JL; Chaussain, C (October 2013). "Extracellular matrix mineralization in periodontal tissues: Noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia". Periodontology 2000. 63 (1): 102–22. doi:10.1111/prd.12029. PMC 3766584. PMID 23931057.
- ^ Boukpessi, T; Gaucher, C; Léger, T; Salmon, B; Le Faouder, J; Willig, C; Rowe, PS; Garabédian, M; Meilhac, O; Chaussain, C (August 2010). "Abnormal presence of the matrix extracellular phosphoglycoprotein-derived acidic serine- and aspartate-rich motif peptide in human hypophosphatemic dentin". The American Journal of Pathology. 177 (2): 803–12. doi:10.2353/ajpath.2010.091231. PMC 2913338. PMID 20581062.
- ^ Reznikov, N.; Hoac, B.; Buss, D. J.; Addison, W. N.; Barros NMT; McKee, M. D. (2020). "Biological stenciling of mineralization in the skeleton: Local enzymatic removal of inhibitors in the extracellular matrix". Bone. 138: 115447. doi:10.1016/j.bone.2020.115447. PMID 32454257. S2CID 218909350.
- ^ McKee, M. D.; Buss, D. J.; Reznikov, N. (2022). "Mineral tessellation in bone and the Stenciling Principle for extracellular matrix mineralization". Journal of Structural Biology. 214 (1): 107823. doi:10.1016/j.jsb.2021.107823. PMID 34915130. S2CID 245187449.
- ^ "Osteomalacia: MedlinePlus Medical Encyclopedia". medlineplus.gov.
- ^ a b Longo, Dan L.; et al. (2012). Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill. ISBN 978-0-07174889-6.
- ^ Kennel, KA; Drake, MT; Hurley, DL (August 2010). "Vitamin D deficiency in adults: when to test and how to treat". Mayo Clinic Proceedings. 85 (8): 752–7, quiz 757-8. doi:10.4065/mcp.2010.0138. PMC 2912737. PMID 20675513.