
Back مشيمة منزاحة Arabic প্লাসেন্টা প্রিভিয়া Bengali/Bangla Placenta prèvia Catalan Placenta praevia German Placenta previa Spanish Aldez aurreko karen Basque جفت سر راهی Persian Placenta praevia French שליית פתח HE Placenta previa Croatian
| Placenta praevia | |
|---|---|
| Other names | Placenta previa |
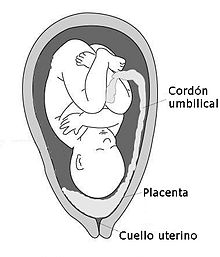 | |
| Diagram showing a placenta previa (Grade IV) | |
| Specialty | Obstetrics |
| Symptoms | Bright red vaginal bleeding without pain[1] |
| Complications | Mother: Bleeding after delivery[2] Baby: Fetal growth restriction[1] |
| Usual onset | Second half of pregnancy[1] |
| Risk factors | Older age, smoking, prior cesarean section, labor induction, or termination of pregnancy[3][4] |
| Diagnostic method | Ultrasound[1] |
| Differential diagnosis | Placental abruption[1] |
| Treatment | Bed rest, cesarean section[1] |
| Frequency | 0.5% of pregnancies[5] |
Placenta praevia is when the placenta attaches inside the uterus but in a position near or over the cervical opening.[1] Symptoms include vaginal bleeding in the second half of pregnancy.[1] The bleeding is bright red and tends not to be associated with pain.[1] Complications may include placenta accreta, dangerously low blood pressure, or bleeding after delivery.[2][4] Complications for the baby may include fetal growth restriction.[1]
Risk factors include pregnancy at an older age and smoking as well as prior cesarean section, labor induction, or termination of pregnancy.[6][3][4] Diagnosis is by ultrasound.[1] It is classified as a complication of pregnancy.[1]
For those who are less than 36 weeks pregnant with only a small amount of bleeding recommendations may include bed rest and avoiding sexual intercourse.[1] For those after 36 weeks of pregnancy or with a significant amount of bleeding, cesarean section is generally recommended.[1] In those less than 36 weeks pregnant, corticosteroids may be given to speed development of the baby's lungs.[1] Cases that occur in early pregnancy may resolve on their own.[1]
Placenta praevia affects approximately 0.5% of pregnancies.[5] After four cesarean sections, however, it affects 10% of pregnancies.[4] Rates of disease have increased over the late 20th century and early 21st century.[3] The condition was first described in 1685 by Paul Portal.[7]
- ^ a b c d e f g h i j k l m n o p "Placenta Previa – Gynecology and Obstetrics – Merck Manuals Professional Edition". Merck Manuals Professional Edition. October 2017. Retrieved 9 December 2017.
- ^ a b Fan, D; Xia, Q; Liu, L; Wu, S; Tian, G; Wang, W; Wu, S; Guo, X; Liu, Z (2017). "The Incidence of Postpartum Hemorrhage in Pregnant Women with Placenta Previa: A Systematic Review and Meta-Analysis". PLOS ONE. 12 (1): e0170194. Bibcode:2017PLoSO..1270194F. doi:10.1371/journal.pone.0170194. PMC 5249070. PMID 28107460.
- ^ a b c Palacios-Jaraquemada, JM (April 2013). "Caesarean section in cases of placenta praevia and accreta". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (2): 221–32. doi:10.1016/j.bpobgyn.2012.10.003. PMID 23127895.
- ^ a b c d Allahdin, S; Voigt, S; Htwe, TT (2011). "Management of placenta praevia and accreta". Journal of Obstetrics and Gynaecology. 31 (1): 1–6. doi:10.3109/01443615.2010.532248. PMID 21280984. S2CID 24852549.
- ^ a b Cresswell, JA; Ronsmans, C; Calvert, C; Filippi, V (June 2013). "Prevalence of placenta praevia by world region: a systematic review and meta-analysis". Tropical Medicine & International Health. 18 (6): 712–24. doi:10.1111/tmi.12100. PMID 23551357. S2CID 22138793.
- ^ Karami, Manoochehr; Jenabi, Ensiyeh (28 July 2017). "Placenta previa after prior abortion: a meta-analysis". Biomedical Research and Therapy. 4 (7): 1071–1078. doi:10.15419/bmrat.v4i07.197. PMID 9396896.
- ^ Baskett, Thomas F.; Calder, Andrew A.; Arulkumaran, Sabaratnam (2014). Munro Kerr's Operative Obstetrics E-Book. Elsevier Health Sciences. p. 178. ISBN 978-0-7020-5248-4.