
Back تشنج المهبل Arabic Vaginizm Azerbaijani Вагінізм Byelorussian Vaginizam BS Vaginisme Catalan Vaginismus Czech Vaginismus German Vaginismo Spanish Tupekramp Estonian Baginismo Basque
| Vaginismus | |
|---|---|
| Other names | Vaginism, genito-pelvic pain disorder[1] |
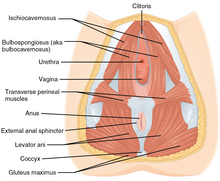 | |
| Muscles included | |
| Specialty | Gynecology, Urology, Sexual Medicine |
| Symptoms | Pain with sex[2] |
| Usual onset | With first sexual intercourse[3] |
| Causes | Fear of pain[3] |
| Risk factors | History of sexual assault, endometriosis, vaginitis, prior episiotomy[2] |
| Diagnostic method | Based on the symptoms and examination[2] |
| Differential diagnosis | Dyspareunia,[4] Vulvodynia[5] |
| Treatment | Behavior therapy, gradual vaginal dilatation[2] |
| Prognosis | Generally good with treatment[6] |
| Frequency | 1-7% of the female population[5] |
Vaginismus is a condition in which involuntary muscle spasm interferes with vaginal intercourse or other penetration of the vagina.[2] This often results in pain with attempts at sex.[2] Often it begins when vaginal intercourse is first attempted.[3] Vaginismus may be considered an older term for pelvic floor dysfunction.[7]
The formal diagnostic criteria specifically requires interference during vaginal intercourse and a desire for intercourse. However, the term vaginismus is sometimes used more broadly to refer to any muscle spasm occurring during the insertion of some or all types of objects into the vagina, sexually motivated or otherwise, including the usage of speculums and tampons.[6][8]
The underlying cause is generally a fear that penetration will hurt.[3] Risk factors include a history of sexual assault, endometriosis, vaginitis, or a prior episiotomy.[2] Diagnosis is based on the symptoms and examination.[2] It requires there to be no anatomical or physical problems (e.g., pelvic floor dysfunction, vulvodynia, vestibulodynia, etc) and a desire for penetration.[3][9]
Treatment may include behavior therapy such as graduated exposure therapy and gradual vaginal dilatation.[2][3] Surgery is not generally indicated.[6] Botulinum toxin (botox), a muscle spasm treatment, is being studied.[2] There are no epidemiological studies of the prevalence of vaginismus.[10] Estimates of how common the condition is are varied.[11] One textbook estimates that 0.5% of women are affected.[2] However, rates in clinical settings indicate that between 5–17% of women experience vaginismus.[10] Outcomes are generally good with treatment.[6]
- ^ Maddux, James E.; Winstead, Barbara A. (2012). Psychopathology: Foundations for a Contemporary Understanding. Taylor & Francis. p. 332. ISBN 9781136482847.
- ^ a b c d e f g h i j k Ferri, Fred F. (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 1330. ISBN 9780323448383.
- ^ a b c d e f "Vaginismus". Merck Manuals Professional Edition. April 2013. Archived from the original on 18 January 2021. Retrieved 15 October 2018.
- ^ Domino, Frank J. (2010). The 5-Minute Clinical Consult 2011. Lippincott Williams & Wilkins. p. 1394. ISBN 9781608312597.
- ^ a b Laskowska, A; Gronowski, P (2022). "Vaginismus: an overview". The Journal of Sexual Medicine. 19 (5): S228-S229. doi:10.1016/j.jsxm.2022.03.520. Retrieved 19 April 2024.
- ^ a b c d "Vaginismus". NHS. 2018-01-11. Retrieved 15 October 2018.
- ^ Yee, Alyssa; Uloko, Maria. "Female Sexual Dysfunction: Medical and Surgical Management of Pelvic Pain and Dyspareunia". Retrieved 19 April 2024.
- ^ Nazario, Brunilda, MD. (2012). "Women's Health: Vaginismus". WebMD. Retrieved December 22, 2016.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Braddom, Randall L. (2010). Physical Medicine and Rehabilitation E-Book. Elsevier Health Sciences. p. 665. ISBN 978-1437735635.
- ^ a b Lahaie M-A, Boyer SC, Amsel R, Khalifé S, Binik YM. Vaginismus: A Review of the Literature on the Classification/Diagnosis, Etiology and Treatment. Women’s Health. 2010;6(5):705-719. doi:10.2217/WHE.10.46
- ^ Cite error: The named reference
Lah2010was invoked but never defined (see the help page).